|
Medical Education Division |
Operational Medicine 2001
Standard First Aid Course
NAVEDTRA 13119



Soft Tissue InjuriesThe most common injuries (trauma) seen in a first aid setting are soft tissue injuries with bleeding and shock. Injuries that cause a break in the skin, underlying soft tissue, or other body membrane are known as a wound. Injuries to the soft tissues vary from bruises (contusion) to serious cuts (lacerations) and puncture wounds in which the object may remain in the wound (impaled objects). The two main threats with these injuries are bleeding and infection. Classification of Wounds Wounds are classified according to their general condition, size, location, the manner in which the skin or tissue is broken, and the agent that caused the wound. It is usually necessary for you to consider some or all of these factors in order to determine what first aid treatment is appropriate. General Condition If the wound is new, first aid consists mainly of controlling the bleeding, treating for shock, and reducing the risk of infection. If the wound is old and infected, first aid consists of keeping the casualty quiet, elevating the injured part, and applying a warm wet dressing. If the wound contains foreign objects, first aid may consist of removing the objects if they are not deep. Do not remove impaled objects or objects embedded in the eyes or skull. Size Generally, large wounds are more serious than small ones and they usually involve severe bleeding, more damage to the underlying tissues and organs, and a greater degree of shock. However, small wounds are sometimes more dangerous than large ones: they may become infected more readily due to neglect. The depth of a wound also is important because it may lead to a complete (through & through) perforation of an organ or the body, with the additional complication of an entrance and exit wound. Location Since a wound can cause serious damage to deep structures, as well as to the skin and tissues below it, the location is an important consideration. A knife wound to the chest is likely to puncture a lung and cause difficulty breathing. The same type of wound in the abdomen can cause a life-threatening infection, internal bleeding, or puncture the intestines, liver, or other vital organs. A bullet wound to the head may cause brain damage, but a bullet wound to the arm or leg, may cause no serious damage. Types of Wounds As the first line of defense against most injuries, soft tissues are most often damaged. There are two types of soft tissue injuries: open and closed. An open wound is one in which the skin surface has been broken, a closed wound is where the skin surface is unbroken but underlying tissues have been damaged. Closed Wounds A blunt object that strikes the body will damage tissues beneath the skin. When the damage is minor, the wound is called a bruise (contusion). When the tissue has extensive damage, blood and fluid collect under the skin causing discoloration (ecchymosis), swelling (edema), and pain. First aid consists of applying ice or cold packs to reduce swelling and relieve discomfort. To guard against frostbite, never apply ice or cold packs directly to the skin. Hematomas are the result of a severe blunt injury with extensive soft tissue damage, tearing of large blood vessels, and pooling of large amounts of blood below the skin. With large hematomas, look for broken bones, especially if deformity is present. First aid consists of applying ice or cold packs to reduce swelling and relieve pain, direct pressure (manual compression) to help control internal bleeding, splinting, and elevation. When large areas of bruising are present, shock may develop. Open Wounds In open soft tissue injuries, the protective layer of the skin has been damaged. This damage can cause serious internal and external bleeding. Once the protective layer of skin has been broken, the wound becomes contaminated and may become infected. When you consider the way in which the skin or tissue has been broken, there are six basic types of open wounds: abrasions, amputations, avulsions, incisions, lacerations, and punctures. Many wounds are a combination of two or more of these types. Abrasions Abrasions are caused when the skin is rubbed or scraped off. Rope burns, floor burns, and skinned knees or elbows are common examples of abrasions. Abrasions easily can become infected, because dirt and germs are usually ground into the tissues. There is normally minimal bleeding or oozing of clear fluid. Amputations Amputations (traumatic) are the non-surgical removal of the fingers, toes, hands, feet, arms, legs, and ears from the body. Bleeding is heavy and normally requires a tourniquet, to control the blood flow. There are three types of amputation: 1. Complete - Body part is completely torn off (severed). If the casualty has an amputation, do the following: 1. Establish and maintain the airway, breathing, and circulation (ABCs). 2. Control bleeding with direct pressure, elevation, indirect pressure, or tourniquet only as a last resort, never remove or loosen a tourniquet once it has been applied. 3. Apply dressing to the stump with an ace wrap to replace direct pressure. 4. Treat for shock. 5. Request medical assistance immediately. Avulsions An avulsion is an injury in which the skin is torn completely away from a body part or is left hanging as a flap. Usually, there is severe bleeding. If possible, obtain the part that has been torn away, rinse it in water, wrap it in a dry sterile gauze, seal it in a plastic bag, and send it on ice with the casualty. Do not allow part to freeze and do not submerge in water. If the skin is still attached, fold the flap back into its normal position. Incisions Incisions, commonly called cuts, are wounds made by sharp cutting instruments such as knives, razors, or broken glass. Incisions tend to bleed freely because the blood vessels are cut cleanly, without ragged edges. The wound edges are smooth and there is little damage to the surrounding tissues. Of all the classes of open wounds, incisions are the least likely to become infected. Lacerations Lacerations are wounds that are torn, rather than cut. They have ragged, irregular edges and torn tissue underneath. These wounds are usually made by a blunt, rather than a sharp, object. A wound made by a dull knife is more likely to be a laceration than an incision. Many of the wounds caused by machinery accidents are lacerations, often complicated by crushed tissues. Lacerations are frequently contaminated with dirt, grease, or other materials that are ground into the wound; they are very likely to become infected. Punctures Punctures are caused by objects that enter the skin while leaving a surface opening. Wounds made by nails, needles, wire, knives, and bullets are normally punctures. Small puncture wounds usually do not bleed freely; however, large puncture wounds may cause severe internal bleeding. The possibility of infection is great in all puncture wounds, especially if the penetrating object is contaminated. Perforation (through & through) is a variation, it is the result of a penetrating object entering, passing through, and exiting the body. Causes Although it is not necessary to know what object or method has caused a wound, it is helpful. Knowing what caused the wound and how it occurred can help you determine its general condition, possible size, type, and seriousness of the wound. This information will help you provide the appropriate first aid to the casualty. Treatment of Wounds First aid treatment for all wounds consists of controlling the flow of blood, treating for shock, and preventing infection. When providing first aid to casualty with multiple injuries, treat the wounds that appear to be life-threatening first. Since most of the body is covered by clothing, carefully examine the entire body for bleeding. When necessary, tear or cut clothing away from the wound because excessive movement of the injured part will cause pain and additional damage. Bleeding After establishing an adequate open airway, the main concern will be to control bleeding, by direct pressure and elevation. Indirect pressure and the use of a tourniquet should be used only if direct pressure and elevation do not control the bleeding. Bleeding control is discussed further in Chapter 3 . A protective covering (dressing) that is properly applied should adequately control the bleeding. In cases of severe bleeding, you may need to double the dressing. Never remove a dressing that is soaked with blood to replace it with another; just place the new dressing over the old one. Shock Shock may be severe in a casualty who has lost a large amount of blood or suffered a serious injury. The causes and treatment of shock are discussed further in Chapter 4. Infection Infections can occur in any wound. Infection is a hazard in wounds that do not bleed freely; in wounds where tissue is torn or the skin falls back into place and prevents the entrance of air; and in wounds that involve the crushing of tissue. Incisions, in which there is a free flow of blood and relatively little crushing of tissues, are the least likely to become infected. The signs of infection are tenderness, redness, heat, swelling, and a discharge. Serious infections develop red streaks that lead from the wound to the heart. Infections are dangerous, especially in the area of the nose and mouth. From this area, (Fig. 5-1) infections spread easily into the bloodstream, causing blood poisoning (septicemia), and into the brain, causing a collection of pus (abscess) and infection. Small wounds should be washed immediately with soap and water, dried, and treated with an application of a mild, non-irritating antiseptic. Apply a dressing if necessary. Make no attempt to wash a large wound and do not apply an antiseptic. Cover the wound with a dry, sterile dressing. Further treatment of large wounds should be conducted by medical personnel. All puncture wounds must be evaluated by medical personnel.
Figure 5-1 Danger Zone for Infection Foreign Bodies Many wounds contain foreign bodies. Wood or glass splinters, bullets, metal fragments, wire, fishhooks, nails, and small particles from grinding wheels are examples of materials that are found in wounds. In most cases, first aid will include the removal of this material if the wound is minor and the object is near the surface and exposed. However, first aid does not include the removal of deeply embedded objects, powdered glass, or any scattered material. Never attempt to remove bullets, examine the casualty to find out whether the bullet remains in the body by looking for both an entrance and exit wound. The general rule is: Remove foreign objects from a wound ONLY when you can do so easily and without causing further damage. Do not attempt to remove an object that is embedded in the eye or that has penetrated the eye. Treatment of Specific Conditions It is impossible to list all wounds in simple categories. Some require special treatment and precautions. You may see wounds that are not described in this course, but most wounds can be treated by calmly remembering the general treatment of wounds. Eye Wounds Foreign bodies such as particles of dirt, sand, paint chips, or fine pieces of metal frequently find their way into the eyes. They not only cause discomfort, but if not removed, they can cause inflammation and infection. Fortunately, through an increased flow of tears, nature dislodges many of these particles before any damage is done. Never let the casualty rub the eye, since rubbing, can cause scratches (abrasions) to the eye and can push a foreign body deeper into the eye, causing further damage. Gently flush the casualty's eye with water at least 15 to 20 minutes. If flushing the eye is not successful in removing the foreign body, patch both eyes and get the casualty to medical personnel. It is always safer to send the casualty to medical personnel than for you to attempt to remove foreign bodies. If the casualty has an object embedded in, or penetrating from, the eye, or the eyeball is protruding from the socket, do the following: 1 .Take a thick dressing or several dressings and cut a hole in the middle, large enough to go over the eye without touching the object. If you cannot cut a hole in the dressing, you can build several dressings around the object. 2. Take a paper cup or other object that is wide enough and strong enough to adequately protect the object without putting pressure on the eye. Place this over the top of the object. Close and cover the unaffected eye to minimize movement of the injured eye. 3. Take a roller bandage and wrap it over the cup and around the head several times ensuring that the cup and dressing are snug enough not to come off, but not tight enough to cause discomfort. When finished, this type of dressing will adequately protect the eye. Laceration of the Eyelids Soft tissues around the eye bleed extensively. This bleeding may make the wound look more serious than it is. However, the bleeding can be controlled easily with a pressure dressing. Before any pressure is applied to the eye, make sure that the eyeball is not cut. If the eye is cut, do not apply pressure to the eye, even to stop bleeding from the eyelid. Pressing on the eye will cause the fluid to leak out, and will result in irreparable damage. If the eyelid is cut and you find fragments of skin, rinse them in water, wrap in a dry sterile gauze, seal in a plastic bag, and send it on ice with the casualty. Do not allow part to freeze and do not submerge in water. If the skin is still attached, fold the flap back into its normal position. When you cover the injured eye you must also cover the good eye. The eyes move together, and even when the injured eye is patched it will move when the good eye moves. Tell the casualty what you are doing, this will reduce their fears of not being able to see. Foreign Objects in the Ear Foreign bodies such as particles of dirt, paint chips, or small insects find their way into the ears. They not only cause discomfort but, if not removed, they can cause inflammation and infection. Never insert anything into the ear to dislodge foreign bodies because you can damage the lining of the ear or cut (perforate) the ear drum. Do not attempt to flush objects out with water; many absorb water and can cause damage from swelling. In the case of insects, if it is alive, shining a light into the ear may attract the insect and cause it to come out. It is always safer to send the casualty to medical personnel than for you to attempt to remove foreign bodies. Head Wounds Injuries to the head (scalp) can occur as a result of diving, automobile accidents, falls, blunt trauma, knives, bullets, and many other causes. Head wounds can be open or closed. In open head wounds there is an obvious injury in which there is normally a lot of bleeding. Closed head wounds may not be obvious, many times you will have to treat the casualty based on how the accident happened. You may see only the delayed symptoms, such as a seizure, confusion, or personality changes. Head wounds must be treated with particular care, since there is always the possibility of brain damage. If you suspect the casualty has suffered a head injury, look for the following: 1. Depressions, lacerations, deformities, bruising around the eyes (Raccoon's Sign) or behind the ears (Battle's Sign). 2. Never touch a wound, examine a wound to determine depth, separate the edges of a wound, or remove impaled objects. 3. Check the eyes: Are the pupils (constricted) small, (dilated) large, equal, or unequal? 4. Blood or clear (cerebrospinal) fluid dripping from the nose or ears. (Cover loosely with a sterile dressing to absorb but not stop the flow). If you suspect a head injury, do the following: 1. Position the casualty flat, stabilize the head and neck as you found them by placing your hands on both sides of the head. 2. Establish and maintain open airway using the jaw-thrust maneuver. Note that the head is not tilted and the neck is not extended. Check the airway, breathing, and circulation (ABC's). 3. Finger sweep to remove any foreign bodies from the mouth. 4. Maintain a neutral position of the head and neck and, if possible, apply a cervical collar or improvised (towel) collar. 5. Control bleeding using gentle, continuous pressure. Never apply direct pressure if the skull is depressed or bone fragments are seen. 6. Apply dressing - Do not use direct pressure or tie knots over the wound. Apply ice or cold packs with cloth to prevent damage to the skin. 7. Treat for shock - Casualtyies with suspected head and neck injuries are to remain flat. Do not raise the casualty's feet. If casualty is vomiting or bleeding around the mouth, place them on their side keeping the neck straight. Do not give anything to eat or drink. 8. Request medical assistance immediately - Time is critical. Facial Wounds Facial wounds are treated, generally, like other flesh wounds. However, ensure that the tongue or soft tissue does not cause an airway obstruction. Keep the nose and throat clear of all foreign material and position the casualty so that blood will drain out of the mouth and nose. Facial wounds and scalp wounds bleed freely. Any casualty that has suffered a facial wound that involves the eye, eyelids, or the tissues around the eye must receive professional medical attention as soon as possible. First aid for other facial wounds is the same as head wounds. Standard First Aid Boxes Non-medical personnel are an important element in providing first aid to casualties prior to the arrival of professional medical personnel. Many lives have been saved by the first aid rendered by a shipmate. Standard first aid boxes are distributed throughout a ship to provide easy access to first aid supplies. The number of first aid boxes and their location depends on the ship's mission and the size of her crew. Various dressings, wire splints, tape, Band-Aids, tourniquets, skin pencils, and other first aid supplies are included in these boxes. Each box is secured with a wire or plastic seal that can be easily broken. The seals are used to identify whether the kit has been opened. A broken seal indicates that the first aid box must be inventoried and restocked. The standard first aid box has three compartments. Each compartment should have a plastic bag that is complete with the basic first aid supplies. Take one of these bags with you on your way to the casualty. Failure to take a bag to the scene may result in you having to go back for supplies. The box does not contain needles, syringes, or medications; but does contain the proper supplies needed to render first aid until medical assistance arrives. First aid boxes are for emergency use only! Report all broken seals to medical personnel as soon as possible. It is important that you know the contents and locations of these boxes. Dressings A dressing is a protective covering for a wound and is used to control bleeding and prevent contamination of the wound. A compress is a sterile pad that is placed directly on the wound. A bandage is material used to hold a compress in place. When applying a dressing, ensure that it remains as sterile as possible. The part of the dressing that is placed against the wound must never touch your fingers, clothing, or any un-sterile object. If you drop, a dressing across the casualty's skin or it slips after it is in place, the dressing should not be used. Battle Dressings Battle dressings are used most often aboard ship and in the field. Each dressing is complete (no other materials are needed) with four tabs which help in applying and securing the dressing. They have "other side next to wound" marked on the outer side. This will help you in (Fig. 5-2) placing the sterile side against the wound. Unless contraindicated, to assist in controlling the bleeding, tie the knot of the dressing over the wound.
Figure 5-2 Battle Dressing Compresses Emergencies may occur when it is not possible to obtain a sterile compress. During these situations, use the cleanest cloth available, a freshly laundered handkerchief, towel, or shirt. Unfold the material carefully so that you do not touch the part that will be placed against the wound. The compress should be large enough to cover the entire wound and extend at least 1 inch beyond its edges. If a compress is not large enough, the edges of the wound will become contaminated. Materials that will stick to a wound or may be difficult to remove should never be used directly on a wound. Absorbent cotton, adhesive tape, and paper napkins are examples of materials that should never come in contact with a wound. Bandages Bandages are strips or rolls of gauze or other materials that are used for wrapping or binding any part of the body and to hold compresses in place. It is not necessary to take time to ensure that the bandage resembles the textbook pictures. However, it is important that the dressing controls the bleeding, prevents further contamination, and protects the wound from further injury. Some of the most commonly used bandages are the roller bandage and the triangular bandage. Roller Bandages The roller bandage (Fig. 5-3) consists of a long strip of material (usually gauze, or elastic) that is rolled and is available in several widths and lengths. Most are sterile, so pieces may be used as a compress on wounds. A strip of roller bandage can be used to make a four-tailed bandage (Fig. 5-4A), by splitting the cloth from each end, leaving as large a center as needed. This type of bandage is used to hold a compress (Fig. 5-4B) on the chin, or (Fig. 5-4C) the nose.
Figure 5-3 Roller Bandages
Figure 5-4 Four Tailed Bandage Triangular Bandages Triangular bandages (Fig. 5-5) are usually made of muslin. They are useful because they can be folded in a variety of ways to fit almost any part of the body. Padding can be added to areas that may become uncomfortable.
Figure 5-5 - Triangular Bandage
Figure 5-6 Cravat Bandage The triangular bandage can be folded to make a cravat bandage, which is useful in controlling bleeding from wounds of the scalp or forehead. To make a cravat bandage, bring the point of the triangular bandage (Fig. 5-6) to the middle of the base and continue to fold until a 2-inch width is obtained. If specially prepared bandages are not available, use whatever material you can find. Remember that the basic purpose of a bandage is to hold the sterile compress in place. Any material or method of application that does not cause further injury to the casualty will be acceptable. Material used as a bandage does not have to be sterile, since it will not come in direct contact with the wound. However, it should be as clean as possible. Cloth bandages should be fastened by tying the ends with a square knot or by tacking the ends with safety pins. If you use a knot to fasten the bandage, be sure to use a square knot. This knot is easy to tie, will not slip, and can be untied quickly. Place the knot so it will cause the least amount of discomfort to the casualty and where it can be removed easily and quickly. Bandages should be applied firmly but not too tight. A loose bandage will slip off the wound. A bandage that is too tight can cut off the blood supply to the injured part and cause damage to the blood vessels and tissues. When you fasten a bandage around an arm or leg, leave the fingers or toes uncovered. If they become blue or swollen, you will know that the bandage is too tight and should be loosened. Figures 5-7 through 5-12 show some of the uses of the roller, triangular, and cravat bandage.
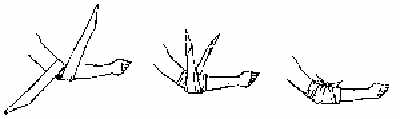
Figure 5-7 - Roller Bandage for the Hand and Wrist
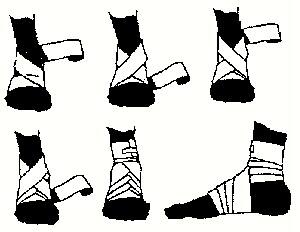
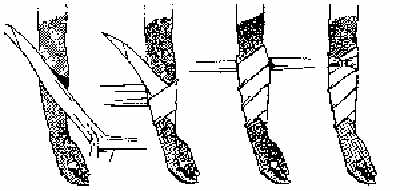
Figure 5-8 - Roller Bandage for the Ankle and Foot
Figure 5-9 - Triangular Bandage for the Head
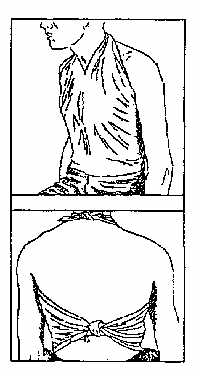
Figure 5-10 - Triangular Bandage for the Chest
Figure 5-11 - Cravat Bandage for the Elbow or Knee
Figure 5-12 - Cravat Bandage for the Arm, Forearm, Leg, or Thigh References 1. NAVEDTRA 10669-C,Hospital Corpsman 3 & 2
Department of the Navy Approved for public release; Distribution is unlimited. The listing of any non-Federal product in this CD is not an endorsement of the product itself, but simply an acknowledgement of the source. Operational Medicine 2001 Home · Military Medicine · Sick Call · Basic Exams · Medical Procedures · Lab and X-ray · The Pharmacy · The Library · Equipment · Patient Transport · Medical Force Protection · Operational Safety · Operational Settings · Special Operations · Humanitarian Missions · Instructions/Orders · Other Agencies · Video Gallery · Phone Consultation · Forms · Web Links · Acknowledgements · Help · Feedback
*This web version is provided by The Brookside Associates Medical Education Division. It contains original contents from the official US Navy NAVMED P-5139, but has been reformatted for web access and includes advertising and links that were not present in the original version. This web version has not been approved by the Department of the Navy or the Department of Defense. The presence of any advertising on these pages does not constitute an endorsement of that product or service by either the US Department of Defense or the Brookside Associates. The Brookside Associates is a private organization, not affiliated with the United States Department of Defense. |